Why Sex-Related Infections Are Spreading Again
Why Sex-Related Infections Are Spreading Again: QuickTake
(Bloomberg) -- Sexually transmitted infections, or STIs, are rebounding in rich countries after being firmly in retreat for decades. Syphilis, for example, can cause stillbirths and infant deaths, and years later can lead to blindness, dementia or paralysis. The resurgence is a result of multiple factors including inconsistent condom usage and the abuse of illicit recreational drugs. At the same time, some common STIs, such as gonorrhea and shigellosis, are becoming harder to treat because of antibiotic resistance. In the U.S., which has the highest rates of sexually transmitted disease in the developed world, the crisis is costing an estimated $16 billion annually in preventable health-care expenses.
1. How bad is the problem?
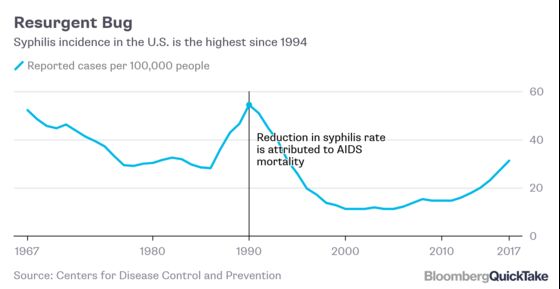
In the U.S., cases of chlamydia, gonorrhea, and syphilis -- three of the most common, treatable sexually transmitted diseases -- jumped by about 10% in 2017 to almost 2.3 million, a record. With syphilis, the annual rate of reported cases in the U.S. has almost doubled in recent years, to 31.4 cases per 100,000 people in 2017 from 15.9 per 100,000 in 2012. The trend with syphilis has also been seen in such countries as France, Belgium, Ireland and the U.K. Reported cases of gonorrhea roughly doubled from 2013 to 2017 in Australia, Belgium, Denmark, Finland, France, Norway, Spain and Sweden. The number of diagnoses in England jumped 26% to a 40-year high last year.
2. What’s driving that?
For one thing, drug abuse. Take syphilis: While the bulk of the roughly 6 million cases occurring annually are in low- and middle-income countries, some of the largest annual increases are in wealthy ones. In these rich countries, syphilis has spread from some high-risk groups, such as gay and bisexual men, to the wider community. In the U.S., rates of early-stage syphilis among women surged 156% from 2013 to 2017. The Centers for Disease Control and Prevention says that’s associated with a corresponding rise in sexualized drug use -- using methamphetamines or injection drugs, including heroin, to facilitate unprotected sex with multiple partners. Similarly in Europe, such practices, known as “party and play” (PnP), “chemsex” or “slamming,” have been shown to spur sex work and risky behavior, especially among men who have sex with men.
3. Are there other factors?
Yes. In the U.S., for example, the decline in AIDS mortality since the mid-1990s has been associated with a rebound in syphilis cases among men who have sex with men. The introduction of drugs to prevent HIV transmission -- called pre-exposure prophylaxis, or PrEP -- has shown great promise in reducing new infections among these men. But it’s also been associated with less consistent use of condoms -- one of the best means of protection against other STIs. More routine STI screening tests among PrEP users has made it difficult to know whether there has been an actual increase, or if previously unrecognized and untreated infections are now being diagnosed. A study from Australia found there was a negligible increase in the STI risk for individuals taking PrEP after controlling for the jump in testing. More international travel and labor migration also mean that germs are spreading faster and wider.
4. What are the consequences?
Each infectious agent presents its own particular dangers. For example, up to 40% of pregnancies in women with untreated syphilis result in miscarriage, stillbirth or early infant death. The surviving babies may suffer from abnormalities including skeletal defects, hearing impairment and meningitis, which can cause developmental delays and seizures. Reported cases of syphilis passed from a mother to her baby have more than doubled in the U.S. since 2013, reaching a 20-year high of 918 in 2017. Florida, California, Arizona, Texas and Louisiana accounted for 70% of cases. With chlamydia, 80% of infections are asymptomatic, yet even then it can be spread via sex. The infection is particularly serious for women. If untreated it may move to the upper reproductive tract, resulting in pelvic inflammatory disease. That can lead to ectopic pregnancy, chronic pain and infertility. Newborns may get pneumonia if they are infected in the uterus. Men with untreated chlamydia may develop arthritis.
5. How serious is drug-resistant gonorrhea?
Very. The bacterium has evolved to thwart multiple antibiotics, leading to at least four reported cases of extensively drug-resistant disease in the U.K. and two in Australia. While the bacterium is broadly susceptible to some newer antibiotics, these appear to be less effective at clearing the infection from the throat. Germs in the throat can spread surreptitiously via kissing, making them harder to stop. A key concern is that ceftriaxone, a backbone of treatment globally, is losing its potency, hastening the threat of untreatable gonorrhea. When the disease isn’t treated, it can cause infertility in both women and men, and potentially lead to a lethal bloodstream infection.
6. What can be done?
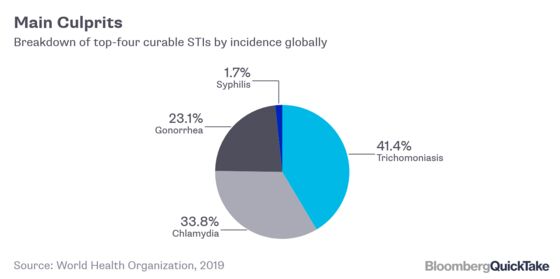
Experience has shown that encouraging condom use isn’t sufficient to curb infections. New tools and therapeutic agents, such as antiviral and antibiotic drugs, are needed. Vaccines, which have significantly reduced cases of human papillomavirus, or HPV, and hepatitis B cases, could be an important defense. Research into vaccines against herpes and HIV is advanced, while immunizations for chlamydia, gonorrhea, syphilis and trichomoniasis, another common STI, are in earlier stages of development.
7. What about the rest of the world?
Most of the more than 1 million people who catch a sexually transmitted infection each day are in low- and middle-income countries. Broadly, STIs are a barometer of access to health care: The worst rates occur in groups least likely to be tested and treated. The World Health Organization recognizes female sex workers, people who inject drugs, men who have sex with men, and transgender women as being most vulnerable. Making available faster and more-reliable tests that can be performed in clinics rather than just in labs would make it easier to detect and treat infections earlier, especially in developing countries and remote areas.
The Reference Shelf
- The U.S. Centers for Disease Control and Prevention’s key resources on sexually transmitted diseases.
- World Health Organization’s global strategy on STIs and its 2018 report on global STI surveillance.
- Why the U.S. National Institute of Allergy and Infectious Disease is prioritizing research in this area and its description of common STIs.
To contact the reporter on this story: Jason Gale in Sydney at j.gale@bloomberg.net
To contact the editors responsible for this story: Michael Patterson at mpatterson10@bloomberg.net, Paul Geitner, Jodi Schneider
©2019 Bloomberg L.P.