How Coronavirus and Race Collide in the U.S.
Black people make up a disproportionate percentage of confirmed Covid-19 cases in the U.S., as do other minority populations.

(Bloomberg) -- The coronavirus originally was touted as a great equalizer in the U.S., with people from every region, race and socio-economic class at risk of contracting Covid-19, the disease it causes. But seven months into the country’s outbreak, it’s clear that Black and brown communities are suffering the most at a time when racial equity is at the forefront of America’s collective conscience.
1. What does the evidence show?
Based on the data that’s available, Black people make up a disproportionate percentage of confirmed Covid-19 cases in the U.S., as do Latinx and other minority populations. Of cases broken down by race and ethnicity as of May 30, Black people made up 22% and Hispanic people made up 33%, according to the Centers for Disease Control and Prevention; these groups constitute 13% and 18% of the population, respectively. The gap between infection rates for Black and White people varies geographically. It is especially wide in some areas, such as Wisconsin, and narrower or non-existent in others, such as Arizona. It’s important to note that the data is spotty and varies state by state. Racial information is available in only 55% of Arizona cases, for instance.
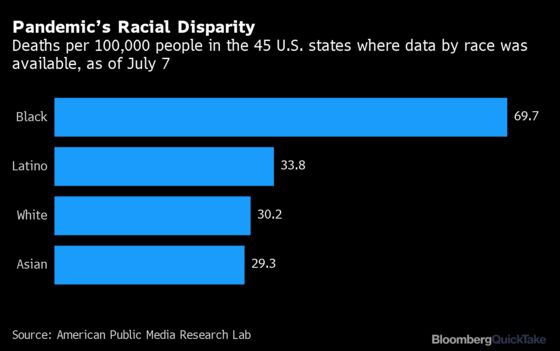
2. What about death rates?
Black and Latinx people are being hospitalized and dying at higher rates than White people, as well as dying at younger ages. One study, not yet peer-reviewed for publication in an academic journal, found the relative death risk to be 3.57 times higher for the Black population and 1.88 times higher for the Latinx community, compared to White people. Again, the gap in hospitalization and death rates varies by location.
3. Why are minority communities more vulnerable?
Black and Latinx people are disadvantaged by discrimination in systems such as housing, education and employment that are meant to support and protect personal well-being. Decades of discrimination have created large wealth gaps between White and Black Americans, limiting opportunities for upward mobility among the latter. Compared to Whites, Black Americans are less likely to have a four-year university degree, are paid less on average, and are less likely to own their homes. These factors put Black Americans at greater danger from the coronavirus, for a number of interconnecting reasons:
- High-risk work. Black and Latinx people are more likely to work in so-called essential jobs, those deemed vital to keeping a society functioning. In 2018, Black Americans made up 36% of nursing, psychiatric and home health aides. A disproportionate percentage of Black employees work in grocery stores, public transit and child care. Because their jobs can’t be moved online, essential workers are exposed to the coronavirus at higher rates and are less able to take time off if they become sick.
- Densely populated housing. Social distancing is critical to slowing the spread of the virus, and Black families tend to live in more densely populated housing than their White counterparts. Black Americans are more likely to live in multi-unit dwellings such as apartments and to have multi-generational households that include older relatives, who are especially at risk of dying of Covid-19. Living in crowded housing is particularly dangerous when family members have to leave the home to work essential jobs.
- Less access to health care. Black and Latinx people are less likely to have access to health insurance and quality health care for a number of reasons, including lack of transportation and child care and discrimination in the health-care system. Black workers are significantly more likely to be uninsured than White workers. Some members of minority groups may decline to seek care because of costs or distrust of health-care providers.
- Higher rates of co-morbidities. Severe complications and death from Covid-19 have been tied to underlying health conditions including diabetes, obesity and heart disease, which are more common in Black people, in part because of inequities in health care.
4. Are there racial disparities outside the U.S.?
Yes, similar trends have been noted elsewhere. In the U.K., Black, Pakistani and Bangladeshi populations are two to three times more likely than the general population to die from Covid-19, according to a study published in May. Barriers to health care and higher rates of pre-existing conditions for those communities are seen as responsible. The Financial Times reported that in Norway, April case numbers showed residents born in Somalia were getting infected at rates well above the national average. Norwegian public health experts posited that a lack of coronavirus information targeted at the Somali community was partially to blame.
The Reference Shelf
- Related QuickTakes on vaccine nationalism, understanding the coronavirus, how the virus spreads, the virus and kids, guidance on masks, and flying in the pandemic.
- A Bloomberg data visualization on race and the virus.
- The U.S. Centers for Disease Control and Prevention discusses race as a factor in the epidemic.
- An interview in Scientific American on the race factor with public health specialist Camara Phyllis Jones.
©2020 Bloomberg L.P.