Add ‘Surprise Billing’ to U.S. Health Care Worries
Add ‘Surprise Billing’ to U.S. Health Care Worries
(Bloomberg) -- A rare point of potential common ground for U.S. President Donald Trump and members of Congress from both parties has emerged on the topic of unexpected medical bills. Much of the debate over health care in America -- which unlike most rich nations doesn’t provide treatment for all citizens -- is what to do about the tens of millions of people who lack coverage. The latest issue to flare involves people who do have coverage, yet still can be financially imperiled by sky-high “surprise billing.”
1. What is surprise billing?
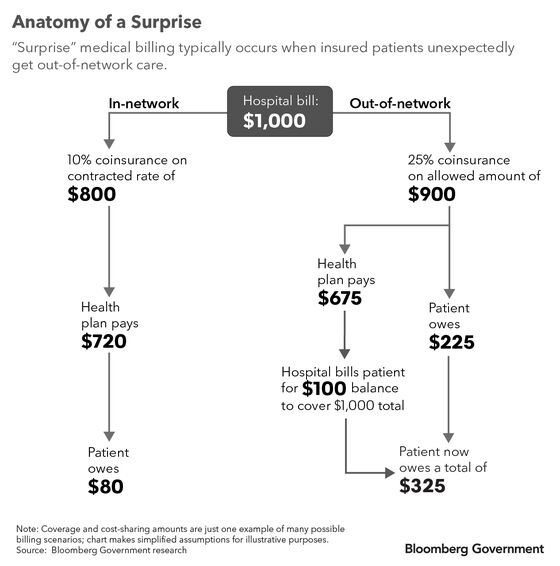
The term generally refers to expensive, unexpected medical bills that patients receive from hospitals and doctors’ offices even when they have health insurance that they expect will cover the majority of the costs of treatment.
2. How can this happen?
Often it’s because the patient got treated by a doctor not on the list of providers that contract with that person’s health plan to provide care at negotiated rates. This can happen on visits to a hospital emergency room, when there’s no option of which doctor to see, for example. Even when patients do seek treatment at a hospital mainly staffed by doctors in their insurance plans, they might wind up being treated by an out-of-network specialist. Worsening the problem, insurers have narrowed their networks of preferred doctors over the years in hopes of steering patients away from hospitals to lower-cost outpatient facilities and doctors. Another issue known as “balance billing” arises when patients are billed the difference between what a doctor charges for a service and what an insurer is willing to pay for it.
3. Is this a common problem?
More than half of Americans say they’ve been surprised by a medical bill they expected would be covered by insurance, according to a 2018 survey by the research group NORC at the University of Chicago. A 2016 survey by the Kaiser Family Foundation found that among insured Americans who say they struggle with medical bills, charges from out-of-network providers were a contributing factor about one-third of the time — and almost 70% of those people said they hadn’t known the health-care provider wasn’t in their plan’s network at the time they received care.
4. What can be done?
There’s a general consensus among lawmakers and even inside the medical industry that people with insurance shouldn’t face unexpected charges because they couldn’t choose the doctor they’d see. The Trump administration wants to require by law that doctors, hospitals and insurers give patients estimates for certain services and alert them before they’re seen by an out-of-network doctor. Insurers want health-care providers to accept typical, usually less expensive, in-network rates. Doctors and other providers argue setting a payment rate based on in-network charges gives too much power to insurers, and they want to use arbitration to seek higher payment rates for their services. New York State has used a similar process since 2015, and it’s resulted in a significant decline in out-of-network medical bills.
5. Why hasn’t anything been done so far?
Congress is caught between health-care providers and insurers over how to settle billing disputes. One proposal from the House tax-writing committee would create a third-party arbitration process for when doctors and insurers disagree over payment amounts. Two proposals from other congressional committees would require doctors who aren’t in a patient’s insurance network to accept the typical in-network rate and allow them to seek arbitration only for bills exceeding a certain threshold.
The Reference Shelf
- Bloomberg Government goes in-depth on the proposals in Congress.
- Vox dug into the problems of surprise emergency-room bills.
- Trump’s support added momentum to the push.
- The Kaiser Family Foundation survey on medical billing problems.
- A Bloomberg Opinion editorial called the problem “scandalous.”
- Unexpected laboratory bills are another issue.
To contact the reporters on this story: Alexander Ruoff in Washington at aruoff2@bloomberg.net;Danielle Parnass in Washington at dparnass@bloomberg.net
To contact the editors responsible for this story: Heather Rothman at hrothman8@bloomberg.net, Laurence Arnold
©2020 Bloomberg L.P.