Covid Stalks U.S. Nursing Homes Again With Virus Redoubling
Covid Stalks U.S. Nursing Homes Again With Pandemic Redoubling
(Bloomberg) -- The coronavirus is cascading into America’s long-term care facilities again in a surge that underscores the nation’s repeated failure to protect its most vulnerable.
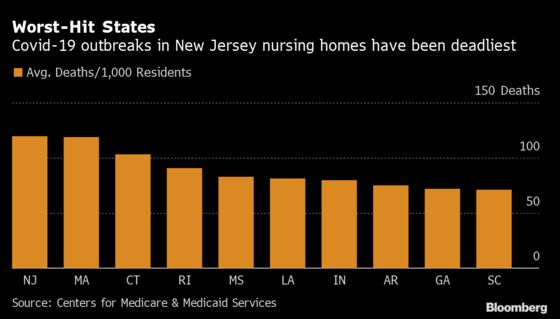
States reported over 29,000 new infections last week in places such as nursing homes and assisted-living facilities, the steepest uptick since at least May, according to Covid Tracking Project data. They come as national daily case counts were higher than ever in November, with a record of more than 170,000 new cases reported Nov. 13. At least 15 states nationwide have already reported single-day record cases this week, including New Mexico, Idaho, and Wisconsin.
On Wednesday, Pfizer Inc. said its experimental vaccine was 95% effective, but developments elsewhere promised months of suffering until the shots are widely available. The nation passed 250,000 deaths, New York City stopped in-person schooling, Wisconsin will extend a mask mandate into next year and news emerged that more than 900 workers at Minnesota’s Mayo Clinic have contracted the virus in the past two weeks. The state’s governor, Tim Walz, said in an evening address that he would shut down much of its economy for a month.

State leaders, public-health experts and owners are sounding the loudest alarms over the spike in nursing homes and long-term care, where cases were falling until September. Meanwhile, visits from families traveling for the holidays threaten to exacerbate the outbreak.
“Our worst fears have come true as Covid runs rampant among the general population,” Mark Parkinson, chief executive officer of the American Health Care Association and National Center for Assisted Living, said in a statement. “Long-term care facilities are powerless to fully prevent it from entering.”

Nursing-home residents often face multiple chronic conditions. More than half of the country’s nursing homes have staff reporting infections, and about 20% have more than 10 victims. Parkinson’s group, which represents more than 14,000 nursing homes and assisted-living communities, said in a report that community spread in the broader population is linked to cases in nursing homes.
In the week leading up to Nov. 12, Ohio reported the largest weekly increase in long-term care cases, accounting for 10% of the national total, according to the Covid Tracking Project. Illinois saw cases double to nearly 2,000 in a week, and Kansas shattered its record. In New Hampshire, four of every five Covid deaths have occurred in a long-term facility.
The data likely underestimate the toll. States vary in reporting: Some lump together resident and staff cases, while others don’t report active outbreaks in facilities at all.
States are grappling with when to pull brake levers, and how hard. Many set harsher lockdowns in November, particularly in the Midwest, where the spread has been sustained and severe. Eight months in, Iowa Governor Kim Reynolds enacted the state’s first mask mandate Monday as cases exploded. Illinois ended indoor dining, museums and casinos, and California reinstituted bans on indoor businesses while warning of a curfew. Minnesota’s Walz on Wednesday night said he would limit social gatherings and close bars and gyms as health-care workers increasingly fall prey to the disease.
In Wisconsin, Governor Tony Evers said Wednesday that he will extend into January a peacetime emergency. “It’s clear, based on where we’re headed, we can’t afford to stop,” he said.
In Kaukauna, Wisconsin, St. Paul Elder Services Inc. experienced two distinct outbreaks at its nursing home since August, said Chief Executive Officer Sondra Norder. Both times, employees who caught the virus in the community brought it into the facility and spread it among patients and co-workers.
In total, 75 residents of about 120 have tested positive, 12 of whom died during coronavirus treatment and eight of whom died after discharge. Since the start of the pandemic, 80 staff members have been infected, 55 from internal spread and another 25 who were exposed outside of the facility.
St. Paul’s outbreaks track with state trends. Cases in Wisconsin picked up over the summer before accelerating after Memorial Day Weekend. Norder is frustrated. She drives past the bar next to St. Paul’s campus on her way home and sees the parking lot packed with cars. At the gas station, she sees people without masks despite signs on the door mandating them.
“This notion that we can protect the most vulnerable in long-term care facilities while otherwise letting the economy and society go on largely as usual with little to no enforceable public-health measures is not working,” Norder said.

The situation is frustratingly cyclical for experts.
“It really has a feeling of deja vu,” said David Grabowski, a professor of health-care policy at Harvard Medical School. Lessons from the first and second spike in nursing homes should have made a third preventable, Grabowski said. But missteps, mainly by the federal government, such as failure to nationalize the equipment supply chain and ensure testing capabilities, have left the elderly and the public at risk again.
Beyond the human toll, repeated spikes threaten to erode the long-term economic health of operators. Occupancy is declining, and short-stay Medicare patients, who are more lucrative, aren’t coming due to the risk, Grabowski said. Combined with added costs for protective gear and testing, the outlook is daunting. “I haven’t heard from a home that isn’t struggling financially,” he said.
In the meantime, the Health Care Association is asking for a litany of assistance measures ranging from a $5 billion testing fund to vaccine priority for residents and staff and enshrined Medicaid protection.
Top Priority
The federal government has made available $333 million for incentives granted to high-performing homes and supplied personal protective equipment. Michael Bars, a White House spokesman, said Wednesday that the administration would prioritize vaccine distribution “to protect the health and safety of elderly Americans in nursing homes and senior living centers.” Bars said it had supplied more than 18 million rapid tests to more than 15,000 nursing homes.
Colorado State Epidemiologist Rachel Herlihy was optimistic about the trajectory of the pandemic in homes. “We’re finding those outbreaks sooner, and that’s largely through the testing strategies that are in place,” she said at a Wednesday news briefing in Denver.
But residents nonetheless remain vulnerable to a disease that seems optimized to harm them.
“There really isn’t a lot that nursing homes could’ve done,” said Tamara Konetzka, a professor at the University of Chicago. “The entire industry is not setup to handle a pandemic.”
©2020 Bloomberg L.P.