Covid Joins War, Cancer as Historic Blight on Americans’ Lives
Covid Joins War, Cancer as Historic Blight on Americans’ Lives
(Bloomberg) -- As 2020 comes to a close, most will remember the year as one defined by sacrifice and loss.
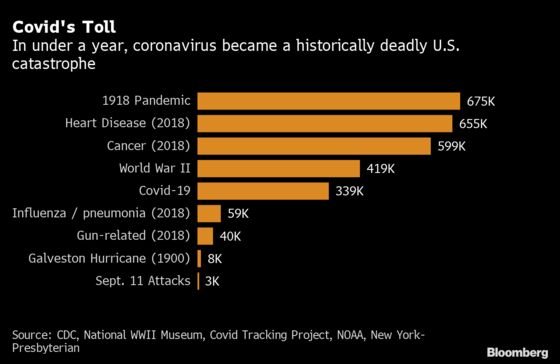
In the 347 days since the first reported U.S. case, the novel coronavirus officially called SARS-CoV-2 bloomed into one of the textbook disasters of modern history. By casualties, the country is mourning the equivalent of a Sept. 11 death toll each day, and is expected to for months. In total, 1 of every 1,000 Americans have died, with heavier burdens on the elderly and people of color.
Among developed nations, the U.S. stands out after a year marred by virus denial, conspiracy, mask politicization and disregard for rules even at the highest levels of government. Stocks touched record highs while millions lost jobs. Even as vaccines are rushed via trucks and planes to those most vulnerable, U.S. hospitals are growing busier by the day.
“I’ve never seen anything like this, to have over 2,000 people die on a day-to-day basis,” said Catherine Kennedy, a registered nurse of 40 years who works at Kaiser Permanente Roseville Medical Center in California. “It’s taken its toll.”
On Wednesday, the U.S. reported 225,671 new cases, bringing the rolling average to 178,740, and setting up the year to close with more than 19 million cases cumulatively, or about one in 20 Americans.
Holiday-season data is affected by a slowdown in testing and reporting, but more broadly, the numbers probably underestimate the caseload. Fewer than 10% of patients with antibodies had been diagnosed in a study published in The Lancet in September.
The death tally, officially more than 340,000, is similarly understated. Some 299,028 excess deaths occurred from late January through early October in the U.S, which are those above the expected total as calculated through statistical models. Two thirds of those are likely attributable to Covid-19, though not counted in the official toll, according to the U.S. Centers for Disease Control and Prevention.
New York City lost its first resident to Covid on March 14, 2020; its total toll is more than 25,000. Mayor Bill de Blasio said Thursday that March 14, 2021, will be a day of remembrance.
“2020 is going to go down in history as one of our saddest, toughest years, arguably the toughest year in the history of New York City,” he said.
The virus sloshed through the U.S. like tainted water, appearing first in the Pacific Northwest, then in the Northeast, South and West before a Midwestern deluge that pushed rural hospitals to their breaking points. Since November, almost every state has broken single-day case records.
New York City on Wednesday reported a seven-day average positivity rate near 8%, the highest in more than seven months. California saw a daily death record Tuesday, and Governor Gavin Newsom said the new highly transmissible U.K. variant had been detected in a patient in Southern California.
The relentless pace of infection, more than 100,000 every day since early November, has weighed on the nation’s healthcare workforce.
Short-Term Fixes
Kennedy’s hospital, northeast of Sacramento, is in the throes of a surge. Capacity is 166 beds, but 244 are in use, thanks to a hodgepodge of short-term fixes -- cramming multiple patients into private rooms and converting underused parts of the building into Covid intensive-care units.
Like many in her position, Kennedy is reusing scarce N95 masks and volunteering for shifts outside her normal job in the neonatal ICU. She worries about the impact on the newest cohort of nurses, and has seen colleagues take stress leave or early retirement.
“We are the richest nation in the world and there is absolutely no reason for it to be like this,” said Kennedy, who is also a president of her state’s nursing association. “The current administration, they failed the people.”
Although treatments have improved and some states have reported patients are generally staying in hospitals for shorter periods, recent waves shifted needs from urban hubs to more rural areas, where resources are scarce. Covid-19 has killed a larger ratio of Americans in rural areas than anywhere else, according to the CDC.
In doing so, the virus exposed the ways the world’s most expensive health care industry has struggled to serve victims. The U.S. spends 17% of its GDP on health care, the most of any major economy, double the average of nations in the Organisation for Economic Co-operation and Development, and in total 42% of global expenditure, according to the World Health Organization. A recent study estimated the impact of the pandemic will slash the U.S. life expectancy at birth by more than a year.
“I did not expect the U.S. to do as shamefully as it has,” said Stephen Bezruchka, an associate teaching professor at the University of Washington School of Public Health, who said the country’s high level of inequality and disjointed state and federal policies have been primary drivers of its failures. “To be honest, I was astounded.”
©2021 Bloomberg L.P.