(Bloomberg Opinion) -- The brutal experience of Covid-19’s first wave humbled many rich countries where even generous health care systems were overwhelmed by an unfamiliar virus. Just as past outbreaks taught Asia hard truths about how to deal with pandemics, lessons from this novel coronavirus abound in the West: Italy has ramped up intensive-care capacity, France is paying health workers better and Spain is building a new pandemic hospital.
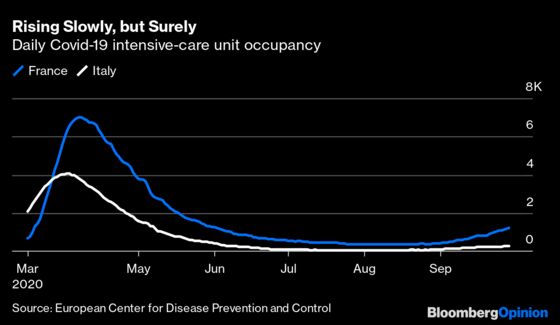
Thanks to these and other efforts, national lockdowns are being portrayed as a one-off. Yet as cases surge again in Europe, strains on critical-care resources are leading to economic shutdowns on local and regional levels.
Covid-19 patients fill more than a third of intensive-care beds in the Paris region. It’s a similar story in Madrid. Blunt, lockdown-style measures — the closure of bars, gyms and other businesses — are being rolled out to slow case growth and hospital admissions. Even though the hospitalization rate is much lower than in the first wave, governments feel they have no alternative but to act now. They’re worried about where that number will be in a month.
France’s Institut Pasteur estimates 11,000 Covid patients could be in intensive care by November. That’s not only above the country’s maximum capacity in a pandemic emergency, but higher than the peak in April.
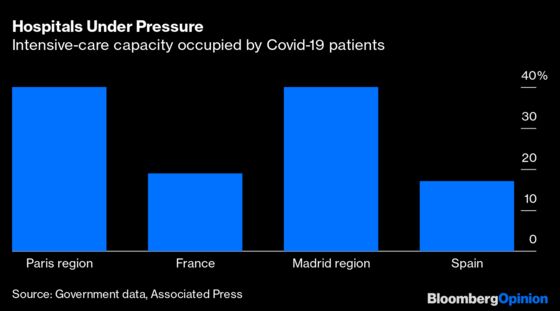
Given hospital metrics feed into governments’ assessment of whether to take tough measures, there’s frustration that so much focus is being put on deciding whether to shut bars or restaurants as opposed to expanding hospital capacity. According to Christophe Prudhomme, an emergency doctor in Paris, if France had structurally doubled bed capacity to 12,000 by now, the national Covid-19 occupancy rate would be around 10% — a level requiring no extra lockdown measures — and not 20%, which does. Are we shutting businesses when we should be building more beds?
The question is more complex than it seems. Intensive-care beds don’t always lend themselves well to cost-benefit analyses in the eyes of government officials. The daily cost of one can be anything from around 2,000 euros ($2,347) to more than double that, according to Rosanna Tarricone, associate professor of health care management at Bocconi University in Milan. You don’t just need a mattress and medical equipment but the staff to operate it. And, crucially, it’s an outlay that may save lives but without countering Covid-19’s spread.
Policy makers therefore face a kind of “Jevons Paradox,” the phenomenon where more supply of a service can increase demand rather than reduce it. Building more beds without getting a grip on the pace of new infections would only serve to fill them up while doing nothing to tackle the core problem. And when epidemics subside, the pressure to cut costs falls on what are suddenly empty beds.
Yet there are limits to strict efficiency analyses in these chaotic times. Governments have shown themselves capable of breaking all sorts of economic taboos, from subsidizing furloughed workers to joint borrowing at the European level. Dismissing hospitals as just another infrastructure “white elephant” looks extreme.
One answer could be to better allocate hospital resources that already exist, rather than permanently increase them everywhere. During Covid-19’s first wave, France used special trains to ship patients around the country, and even across the border to Germany and Luxembourg. Cross-border cooperation makes even more sense now, with some countries being hit hard, while others such as Italy or Germany fare much better. Philippe Juvin, head of emergency services at Paris’s Europeen Georges-Pompidou Hospital, has proposed creating a European reserve of medical staff and resources that could be sent from less affected countries to those facing saturation.
Another way to ease the strain on intensive-care units can involve reorganizing hospitals themselves. South Korea, which resisted Covid-19 lockdowns via extensive surveillance and testing, used its playbook from the 2015 MERS coronavirus outbreak to allocate patients based on symptom severity and bed availability. Patients were shared among community facilities, dedicated Covid-19 hospitals, and other locations. The community facilities, for instance, housed patients who reported their body temperature and any symptom changes using a mobile app or the telephone while they were there, making any on-site responses and eventual hospital transfer easier.
This would require rethinking how resources are used in a way that doesn’t come easily to Western countries that were spared deadly pandemics for decades. It’s also not a substitute for preventative measures. Test-and-trace systems have approached the brink of collapse in several countries — they could also do with European common standards and technology for contact-tracing apps, for example.
Still, if ever there was a time to view health care as a benefit to society and the economy, rather than a drag on public finances, it’s now. If we want to learn to live with the virus, we should think about hospital beds, not just bars.
This column does not necessarily reflect the opinion of the editorial board or Bloomberg LP and its owners.
Lionel Laurent is a Bloomberg Opinion columnist covering the European Union and France. He worked previously at Reuters and Forbes.
©2020 Bloomberg L.P.