U.S. Vaccinations at 200,000 a Day Run Far Short of ‘Warp Speed’
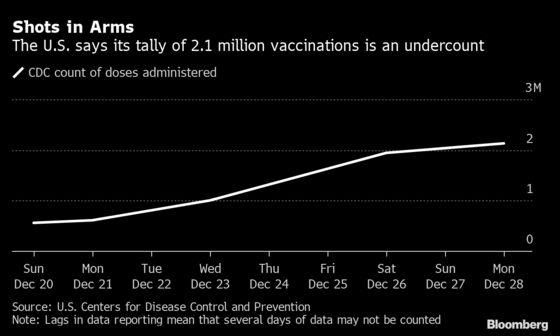
The U.S. is vaccinating an average of only 200,000 people a day against Covid-19.

(Bloomberg) -- The U.S. is vaccinating an average of only 200,000 people a day against Covid-19, and many states have used just a small percentage of the shipments sent to them this month.
Data gathered from states and the U.S. Department of Health and Human Services show that while Operation Warp Speed has distributed millions of doses, some states have been slow to get them into people’s arms. The nation almost certainly won't hit the Trump administration’s goal of 20 million vaccinations by year-end, according to a Bloomberg News analysis.
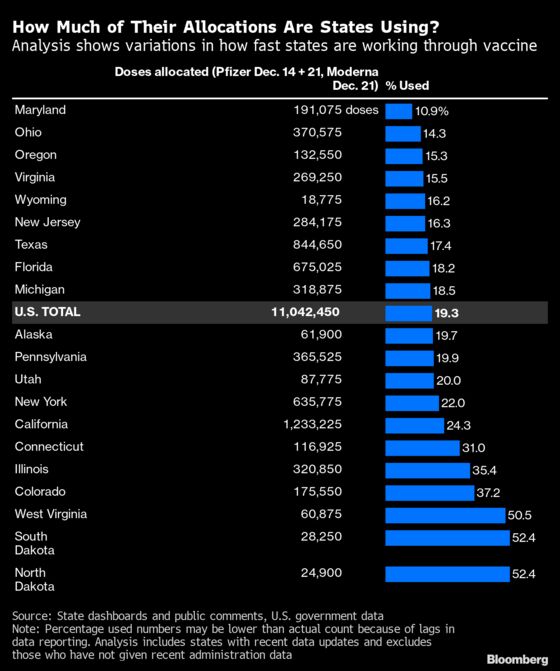
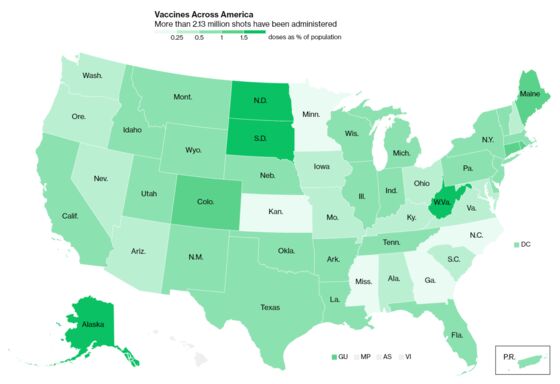
The CDC’s latest tally, as of Monday, showed that despite the distribution of 11.45 million doses from Moderna Inc., and from Pfizer Inc. and BioNTech SE, just 2.13 million people had gotten shots. That represents about 20% of early allocations. Oregon has used only 15.3% of its supply, Ohio 14.3% and Maryland 10.9%.
Officials blame a delicate vaccine with complex storage requirements, uncertainty over the supply of doses and strain on local health agencies already facing historic challenges.
“We would like to have better uptake,” said Steve Kelso, a spokesman for the Kent County Health Department in Michigan, where the state has used 18.5% of its doses. “We could be sticking more needles in arms."
More than 330,000 Americans have died from the pandemic and tens of thousands more are expected to succumb in coming months, making the vaccine’s rollout all the more critical. But Moncef Slaoui, chief science advisor to Operation Warp Speed, said last week that the goal of getting 20 million people vaccinated by year-end was unlikely to be met.
In recent weeks, countries around the world have launched vaccination campaigns in a global race to end the pandemic. Some are far outstripping the U.S.: Israel, whose size and population is similar to New Jersey’s, gave shots to an average 60,000 people a day in its first week. If the U.S. were moving at the same speed, it would be doing 2.2 million daily inoculations — 10 times its current pace.
A Health and Human Services Department spokesman said Tuesday that reported numbers don’t reflect the latest situation.
“We are closely monitoring the data being reported from the jurisdictions about vaccine administration, and we are encouraged by the work they have done so far during the holidays,” said Michael Pratt. “There is an expected lag between shots going into arms and the data being reported.”
President Donald Trump on Tuesday evening reiterated in a tweet that “it is up to the States to distribute the vaccines. He reiterated the sentiment again on Wednesday morning, telling states to “Get moving!”
But President-elect Joe Biden said in an earlier speech that “the effort to distribute the vaccine is not progressing as it should” and that he would “move heaven and Earth to get us going in the right direction.”
Biden said his administration would achieve 100 million shots in his first 100 days if Congress provides funding. “If it continues to move as it is now, it’s going to take years, not months, to vaccinate the American people,” he said.
Michigan’s Muddle
Bloomberg News analyzed the first three allocations to states, including two weeks of Pfizer shots and one of Moderna's. In some cases, the totals allocated are higher than what states say they have received. The number of doses shipped aligns with what the CDC says has been distributed, allowing consistent state-by-state comparisons.
Michigan has used less than 1 in 5 of its 455,900 doses allocated through Dec. 21, according to Bloomberg’s analysis.
“The lack of certainty about vaccine allocations, timing of those allotments arriving and the process of scheduling thousands of employees for vaccination have all made it challenging,” said John Karasinski, spokesman for the Michigan Health & Hospital Association.
Kent County, which encompasses Grand Rapids, formed a group of health departments, hospitals and pharmacies with the goal of vaccinating about 2,200 people in the first phase, which targets health workers. So far, it's done only about 575 vaccinations.
Kelso, the spokesman, said some employees don't want to deprive a true front-line worker of a vaccine. The holidays may be slowing things. And some people are still skittish about safety, even some of the health department staff.
“A lot of people don’t want to be the first kid on the block,” Kelso said.
Other groups are having more success. Sparrow Health System has vaccinated about a quarter of its staff, Pharmacy Director Todd Belding said in an interview. The central Michigan hospital system is administering about 2,000 doses per week, about as much as its allocation from the state, he said.
The staged rollout is slower than if the shots were available to all comers, like the flu vaccine. Some delay is by design: Hospitals don't want to vaccinate entire departments at once, in case side effects force workers out. But Sparrow is also coordinating with officials to target populations like prison medical staff and independent health-care practitioners. Identifying and reaching such groups takes time, a challenge that will persist when vaccines trickle down to grocery workers and teachers.
“That prioritization has added kind of a level of complexity,” Belding said.
Other states are moving more slowly. As of Dec. 28, Maryland had worked through only 10.9% of its 191,075 doses from the first three weekly allocations, according to Bloomberg's analysis.
In Montgomery County, Chief of Public Health Travis Gayles said he's preparing for obstacles like staffing shortages. Years of budget cuts kneecapped municipalities' ability to build effective virus responses from scratch — at one point, Montgomery was tallying virus cases by fax — and those cuts may hobble vaccine distribution as well.
"With Covid right now, it definitely shows a bright light on the impact of those budget decisions," Gayles said.
In New York, officials are watching vaccination sites and giving “gentle pressure to pick it up,” said Larry Schwartz, a member of Governor Andrew Cuomo’s Covid-19 Task Force. A portion of the state’s allocation goes to pharmacies that the federal government hired to inoculate nursing-home residents and staff, and it may have taken them time to gear up, Schwartz said.
“Like anything that’s totally brand new, there’s always a little bit of a ramp-up period,” he said.
Ashish Jha, dean of Brown University’s School of Public Health, said the Trump administration’s reliance on states has hamstrung the response. The Warp Speed program succeeded admirably in helping develop and distribute a vaccine, he said, “but at that point it’s hitting a roadblock.”
“Let’s set up field hospitals and tents everywhere and have the National Guard do this,” Jha said in a telephone interview. “That last mile has gotten very little investment. I think this is going to be a huge problem.”
Private institutions are struggling, even those performing relatively well. In Virginia, which overall has used about 15% of its early allocation, Sentara Healthcare has given about 60% of its doses, said Jordan Asher, chief physician executive of the 12-hospital system. The internal goal was to distribute that in three weeks, and Asher said Sentara was slightly ahead of schedule.
Complexity nonetheless slows things down. Sentara is receiving doses at its main hospital in Norfolk, then bringing some by freezer truck to other medical centers. Supply has to be precisely matched with staff ready and scheduled to take the shots, to ensure none are wasted and they’re given to priority groups.
“You’re trying to deal with a pandemic crisis on hospital beds, and at the same time you’re trying to do a brand-new vaccination program that is unlike anything we’ve had to do before,” Asher said.
Congress appropriated $8.75 billion this week for the vaccination effort, more than half of which will go to states. But Jason Schwartz, an assistant professor at the Yale School of Public Health, said existing health infrastructure simply isn’t designed to do millions of vaccinations a day.
“It’s only going to get harder as we scale up and scale out,” he said.
©2020 Bloomberg L.P.