Medical Debt Is Crushing Black Americans, and Hospitals Aren’t Helping
Medical Debt Is Crushing Black Americans, and Hospitals Aren’t Helping
(Bloomberg Businessweek) -- Tango Walker estimates her family owes more than $28,000 in medical debt. Her five active kids often got banged up playing sports and needed minor surgery or physical therapy. She still owes money for an $1,800 custom knee brace her daughter, now a college junior on a basketball scholarship, got after tearing her ACL in 10th grade.
Walker, who has a master’s degree in educational leadership and is working toward a doctorate, recently started a job at the Children’s Advocacy Center at the University of Missouri at St. Louis. Even with insurance, she struggles to afford care. Last year she was surprised to learn her wages had been garnished with no notice for a surgery bill she didn’t know about.
She says she’s never been offered the financial assistance she later learned is often available, even though nonprofit hospitals are required by law to publicize charity-care policies. Walker, who’s Black, sees a double standard. “I’ve witnessed how White people are spoken to and how things are explained to them as opposed to how I’ve been spoken to and how things have been explained to me,” she says.

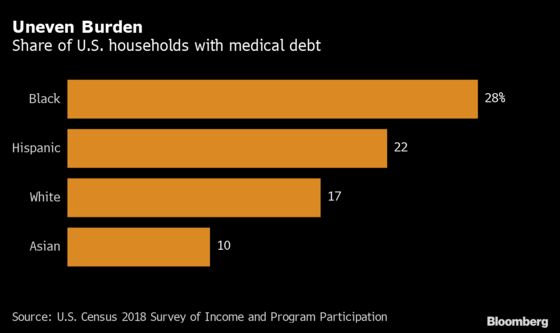
Walker’s debt is part of an enormous burden of $140 billion in past-due medical bills reported on U.S. credit files. But that burden isn’t evenly distributed: It disproportionately falls on Black Americans. Census data show that 28% of Black households have medical debt, compared with 17% of White households.
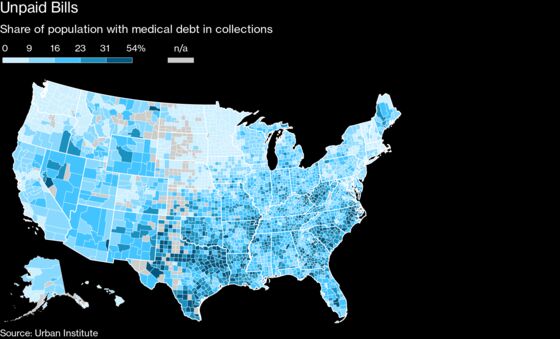
The gap is even wider in certain parts of the country. In St. Louis County, where Walker lives, people living in communities of color are almost four times as likely to have medical debt in collections than people living in predominantly White communities, according to data compiled by the Urban Institute.
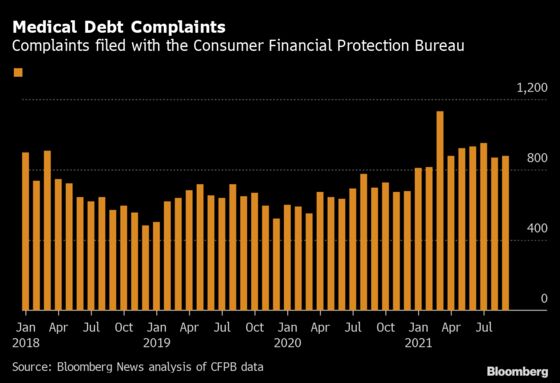
Hospitals have performed heroic work to save lives amid the immense challenges of the Covid-19 pandemic. Through it all, many institutions continued to pursue collection of medical debt. After George Floyd’s murder last year and the protests that followed, hospital groups and medical societies pledged to advance racial equity. The American Hospital Association called for “the hard but necessary work to make fundamental changes and address our society’s inequity,” and “real solutions that make a genuine difference.”
Health-care companies can’t fix the root causes of the country’s systemic inequality, but doctors and hospitals can ensure their services don’t inflict financial harm on patients. For instance, they can determine how to screen patients for financial assistance and how to respond when a bill goes unpaid. But patient advocates say the medical industry perpetuates such harsh billing practices as garnishing wages, charging high interest rates, placing liens on homes, and suing patients. Those tactics often land harder on communities of color.
Meanwhile, these aggressive billing practices bring in little revenue for hospitals—less than 1% of the total by some estimates, patient advocates say. “These are already people who’ve been struggling to pay,” says Jenifer Bosco, a staff attorney at the National Consumer Law Center who co-wrote proposed legislation to strengthen protections for patients. “It’s not the way the hospitals are balancing their budgets.”
Hospital industry groups have opposed state legislation intended to shield patients from harsh collections practices. Yet complaints about medical collections filed with federal authorities have persisted through the pandemic, the protests that followed Floyd’s murder, and beyond.
Most U.S. hospitals are nonprofits or public entities; only about a quarter are for-profit companies. Consumer advocates say that as tax-exempt organizations, health-care systems should ensure that patients eligible for financial help don’t get passed to debt collectors instead. They want medical providers to make clear to patients what assistance is available and halt the practice of garnishing wages or putting liens on houses. And they’re pressuring hospitals to more broadly reexamine the impact of billing and collections tactics on communities of color. Those practices, they argue, are especially punitive in the context of the $119 billion in taxpayer money doled out to stabilize hospital finances upended by the pandemic.
“We invest a lot in our nonprofit hospital systems, and in exchange we ought to be able to expect them to behave like charities,” says Elisabeth Ryden Benjamin, vice president for health initiatives at the Community Service Society of New York, a consumer group that fields health-care questions and complaints on behalf of the state.
In response to a rising number of complaints about medical billing, Benjamin’s group analyzed almost 31,000 debt-collection lawsuits filed by New York state’s hospital systems over five years. The median debt was $1,900. The results surprised her: Most of the litigation seeking debt repayment came from a handful of big nonprofit health systems, while dozens of other hospitals never brought suits.
NYC Health + Hospitals, which calls itself the largest public health-care system in the U.S., was among those that brought suits, though it was far from the most litigious. Benjamin was alarmed to find hundreds of lawsuits filed by the city’s main safety-net provider. In a meeting in 2019 she asked the system’s chief executive officer, Mitch Katz, about them.
Katz was surprised, too. He didn’t know about the lawsuits. “I thought that was unacceptable, and so we ended all of those suits,” he says in an interview. “We’ve been known to sue insurance companies, but we don’t want to sue our patients.” NYC Health + Hospitals has always provided free and low-cost care, Katz says, but some patients didn’t apply or didn’t know they could apply. Some undocumented immigrants may fear volunteering the information needed to qualify. The health system has boosted its outreach and extended the hours its financial counselors work. Those changes are intended to make charity care more accessible. “If we have a bill, we proactively contact them and say, ‘Did you know that you are eligible?’” Katz says.
Benjamin also got a meeting with leaders from NewYork-Presbyterian, another one of the city’s largest health-care systems. They didn’t renounce lawsuits as NYC Health + Hospitals did, but they did instruct their collections agency to stop charging a 9% interest rate, Benjamin says. A spokesperson for NewYork-Presbyterian says the hospital doesn’t charge interest on patient judgments but didn’t comment on the rest of Benjamin’s account.
Other health-care systems, including Northwell Health, the state’s largest, have been less receptive to change, Benjamin says. Northwell representatives say that the system resorts to lawsuits only if patients don’t respond to outreach, including offers of financial assistance, and that it has paused lawsuits during Covid.
For Benjamin, the meetings were revealing. “In some cases, hospitals didn’t know what they were actually doing,” she says. “There’s something going on where it’s on autopilot for these systems.” Indeed, a November report by Benjamin’s group revealed that New York hospitals filed thousands of liens against patients even as they collected state funds intended to cover the care of people who can’t pay.
It’s hard to separate the disparities in medical debt from other inequities. Black and Hispanic households are more often uninsured than White and Asian households, and they have lower incomes and less wealth to absorb unexpected shocks like medical bills.
Still, racial gaps in medical debt aren’t inevitable. Massachusetts, Minnesota, Washington, and other states have low levels of medical debt and narrow differences in debt levels measured by race, according to Urban Institute data. In other areas, including much of the South, where states haven’t expanded Medicaid eligibility, debt is more common, and the gaps between White communities and communities of color are wider.
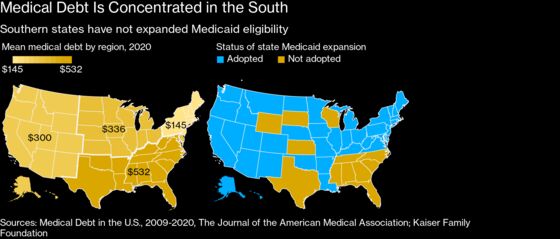
Congress is weighing whether to expand insurance coverage directly in those states as part of President Joe Biden’s economic plan passed by the House on Nov. 19. The change could bring coverage to 2.2 million, about 60% of whom are people of color, according to a recent Kaiser Family Foundation analysis. Meanwhile, advocates are campaigning to strengthen legal protections for patients by forcing disparities into the spotlight.
In Baltimore, Ashley Esposito, an IT worker for the state of Maryland, testified at a virtual hearing earlier this year in favor of a bill to limit medical debt collections practices. Esposito, 37, unwittingly accrued about $2,000 in debt during fertility treatments at Johns Hopkins clinics. While some of the treatments were covered by her health plan, Esposito, who’s Black, owed fees she says she was never asked for at her visits.
She discovered the charges only when debt collectors started calling after her son was born in the summer of 2020. “She was treating me like I was a criminal,” says Esposito of one debt collector. “I stopped taking the calls, because I was literally trying to recover from a C-section, take care of a baby,” and work from home during the pandemic.
Esposito and her husband are carriers of a rare genetic condition that led to two failed pregnancies, and she says she has nothing but praise for the doctors at Johns Hopkins who helped them have a healthy child. But the experience with the collections agency left her angry. It also brought to mind instances of racism Esposito had encountered getting medical care.
She recalled visits with doctors elsewhere who directed questions to her husband, who’s White, that they both thought should’ve been posed to her. White friends who saw the same doctors received different care, she says, and she worried her concerns during difficult pregnancies weren’t heard.

“Who’s to say that doesn’t carry over into the financial piece? That those same implicit or explicit biases don’t carry over?” Esposito asks. “If it’s disproportionately happening to people of color, there’s already a fear of not being treated fairly or receiving good-quality treatment.”
Johns Hopkins declined to comment on Esposito’s account. State law requires hospitals to seek payment from patients who can pay, a spokesperson said in an email, and patients typically get “multiple opportunities to file for medical or financial hardship” before bills are sent to collections. The hospital paused debt collection lawsuits against patients in 2020 and takes “extensive steps” to help patients understand financial assistance and payment options, the spokesperson said.
Joseph Fifer, the leader of the Healthcare Financial Management Association (HFMA), a professional group for health-care finance workers, says hospitals can do better. In a column earlier this year, he urged the profession to review practices for implicit bias and question whether financial assistance and counseling are equally available to all patients. Last year, the HFMA published voluntary best practices on collecting payments. Among many recommendations, the document suggests hospitals analyze the percentage of patients by race whose accounts are written off as bad debt and who are subject to aggressive collections actions such as liens or lawsuits.
The American Hospital Association has also promoted voluntary guidelines on patient billing, updating them since Covid. The document suggests hospitals refrain from reporting debts to credit bureaus, suing patients, or garnishing wages unless they’ve established that a patient “is able but unwilling to pay.” One sign of change: The number of financial assistance transactions processed by TransUnion Healthcare, a subsidiary of the credit reporting agency, has increased 50% to 60% annually since the company started tracking them three years ago.
In Maryland, hospitals are required by law to provide free care to patients making less than 200% of the federal poverty guidelines, or an income of $53,000 for a family of four. But 60% of hospitals’ unpaid charges to people in that income bracket were reported as bad debt, according to a state report, suggesting “that hospitals attempted (and failed) to collect this debt from a sizable number of patients likely eligible for free care.”
Marceline White, the leader of the Maryland Consumer Rights Coalition, says the state’s hospitals were three times more likely to sue patients in low-income areas. The median debt hospitals sued over was $944, according to an analysis, compiled by the coalition and labor groups, of 145,000 lawsuits over 10 years. As in New York, the Maryland analysis showed a wide variation in hospitals’ willingness to pursue debts in court.
The group has uncovered racial disparities as well. In a poll it commissioned, just under half of African-American respondents said they were aware that hospitals provided free or low-cost care for low-income patients. Among White respondents, 79% said they knew about the programs. “There are a lot of patients who don’t know that that’s available,” White says.
Advocates and labor groups, including the National Nurses United union, have been pushing lawmakers to expand patient protections. Maryland enacted a law this year that will keep hospitals from putting liens on patients’ homes or garnishing the wages of people who qualify for charity care. It will also require hospitals to report to the state about the debts they’re suing over, including data on race and ethnicity of debtors. That should shed more light on whether the practices contribute to racial disparities, White says. She called it “the strongest medical debt protection bill in the country.” The state’s hospital association initially opposed the law before changes were made.
Other states are taking action, too. A Colorado law enacted this summer aims to standardize how health-care providers screen patients for financial assistance and puts additional strictures on collections practices. A New Mexico law bars collections against people under 200% of the poverty level. And in California, a new law will raise the income ceiling under which patients are eligible for charity care and restrict hospitals’ ability to sell debts to debt buyers.
None of that will help Tango Walker, whose lingering medical debt continues to take a toll on her family in St. Louis. “It really can alter someone’s entire ability to live,” she says, pointing to the endless trade-offs she’s forced to make. “Do I get this medication that my child needs or pay the electric bill?”
©2021 Bloomberg L.P.