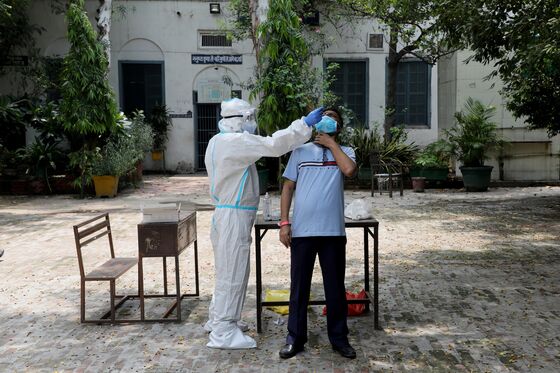
India’s Flimsy Virus Testing Regime ‘Like Flipping a Coin’
India’s bid to control its surging infections by increasing the use of fast but less sensitive tests could be making things worse

(Bloomberg) --
India’s bid to control its surging virus infections by increasing the use of fast but less sensitive tests could actually be making things worse for the South Asian nation.
With one of the world’s fastest-growing epidemics but also one of the lowest testing rates, India in late June started to use quick antigen tests to ramp up detection. But the tests, which can report false negatives as much 50% of the time, threaten to obscure the true picture of its outbreak, further challenging containment efforts.
Between 25-30% of the country’s daily tests now are rapid antigen tests, Balram Bhargava, the director general of the Indian Council of Medical Research, told reporters at a briefing in New Delhi. It was the first time India’s premier research group had broken down the testing data -- the ICMR’s website still does not specify what type of tests are being done in its daily data.
In some cities like capital New Delhi, the rapid testing numbers are even higher -- the latest data as of Aug. 12 showed the city conducted 12,422 rapid antigen tests and 6,472 of the more sensitive real time-polymerase chain reaction tests.
The reliance on these tests casts further doubt on the ability of Prime Minister Narendra Modi’s government to stem the epidemic, which is now surging unchecked through the nation’s hinterland. It may also mean the falling case numbers seen in its big cities could be due to false negatives, raising questions over whether infection is truly being curbed.
Worse, the use of rapid tests could be letting some infected people return freely to the community, spreading the pathogen to even more people. In the Philippines, a high number of false negatives on tests conducted on returning workers meant that infections were seeded in new places when they were allowed to go home, sparking a fierce resurgence of cases.
India’s federal health ministry didn’t respond to an email and a phone call seeking comment.
Most other countries with big outbreaks like the U.K. and the U.S. use the RT-PCR tests that detect the genetic material of the virus. While experts say that rapid antigen tests can help countries with out-of-control outbreaks quickly detect where hot spots are, India’s practice of conflating the data from rapid tests and traditional RT-PCR ones risks obscuring its true infection picture.
Other tests, like those for serological studies or testing high risk groups for antibodies, are counted separately. The U.S., whose testing protocol was recently slammed by Microsoft Corp. founder and billionaire philanthropist Bill Gates, hasn’t managed to scale up its testing facilities to push through as many tests as it needs to.
“I don’t think it’s good science to put together the two tests. If the rapid antigen tests are only 50% sensitive compared to PCR tests and there is a very high prevalence of community transmission then they are not very good test,” said Peter Collignon, a professor of clinical medicine at the Australian National University Medical School. “Flipping a coin might almost be as good.”
Shifting Strategies
The quicker test itself isn’t the problem. Rapid antigen testing is viewed as a competent strategy to test widely -- it’s faster, cheaper and requires less complex technology than molecular testing. The rapid tests cost about 450 rupees ($6) compared to the molecular tests, where the government has capped the price at 2,400 rupees.
“The basic approach should be to test as widely as possible, but to report results separately for RAT and RT-PCR so that trends in each can be studied separately,” said Prabhat Jha, professor of Global Health and Epidemiology at the Dalla Lana School of Public Health, University of Toronto.
In Asia the countries that have had the most success in controlling their infections, like China and South Korea, don’t use the rapid tests much because they scaled up their molecular testing capacity early on.
The World Health Organization’s guidance, unchanged since April, has been to use the more accurate PCR tests.

Opaque Data
India’s clubbing together of its different types of tests is part of the nation’s bigger problem with opaque data and one that experts say hinders its pandemic battle.
Delhi Chief Minister Arvind Kejriwal has suggested the capital is moving toward herd immunity after a serological survey last month found antibodies in 23% of the samples tested. Experts warn this is an unreasonable projection, especially given the brief press release gave scant details about the tests themselves.
The results of a similar survey, using antibody testing, conducted earlier by the ICMR have yet to be released.
Jha believes the details of the Delhi antibody test need to be published for independent scientific scrutiny and described the suggestion that herd immunity is developing as “scientifically suspect.”
“The key here is not the test. It’s the reporting and sharing data on individual records (protecting confidentiality) as well as say Singapore did,” Jha said in an email. “Without open data, India will struggle more to curb the virus.”
©2020 Bloomberg L.P.