Hospitals Deluged as Vaccine Still Months Away for Most in U.S.
Hospitals Deluged as Vaccine Still Months Away for Most in U.S.
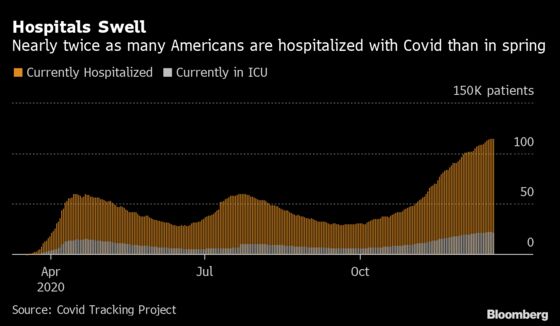
(Bloomberg) -- Covid-19 has hospitalized almost twice as many Americans as at any point in the pandemic, leaving medical providers on the brink of crisis with vaccine doses months away for most people.
The U.S. health-care system and those who serve it are enduring more strain than ever. And the virus’s grip on hospitals has shifted toward more rural communities, where treatment alternatives are scarce.
In the near term, sustained patient loads threaten to accelerate deaths, as access to critical care declines in intensive-care units. Longer term, the risks are more systemic: fatigue, attrition and mental-health damage to the doctors and nurses working to care for the sick.
“The moment when the percent of beds occupied by Covid patients increases, that really drives a lot of the staffing issues,” said Pinar Karaca-Mandic, a health-care risk management professor at the University of Minnesota. “It exposed a lot of the fragmentation in our health-care system.”
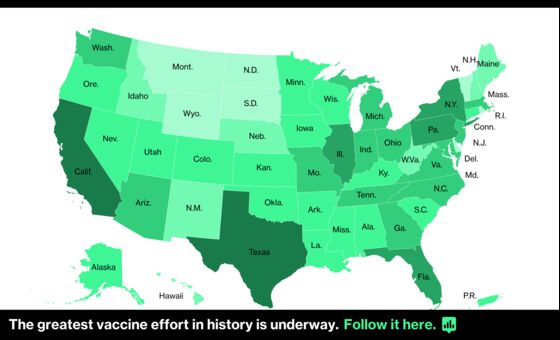
More than 115,000 Americans are currently hospitalized with coronavirus, according to Covid Tracking Project data -- a number that has risen alongside daily cases since early October. California, Texas and New York account for more than a quarter of the national total.
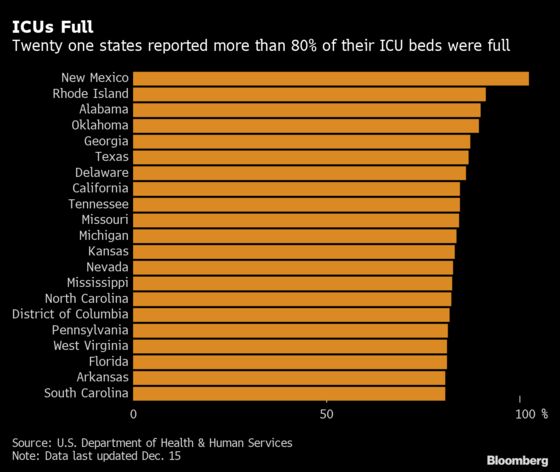
Almost one in five U.S. hospitals reported critical staffing shortages on Friday, according to data from the Department of Health and Human Services. Earlier this month, HHS released figures that gave a more localized view of the devastation, which was previously obscured by national or statewide numbers.
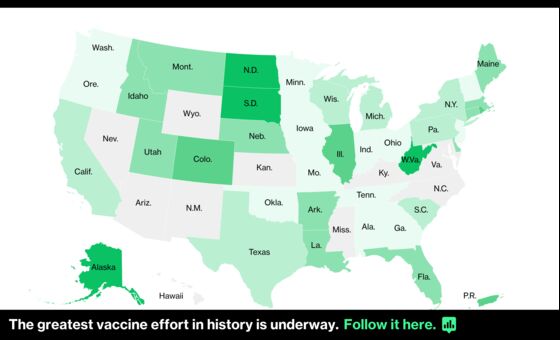
Non-metro areas are suffering more in the current wave, with larger occupancy rates than more densely populated regions, said Karaca-Mandic, whose team analyzed the data.
More than a dozen counties -- such as Burke, North Carolina, and Hale, Texas -- reported at least 90% of their ICU beds filled by Covid-19 cases, leaving hardly any capacity to treat others. Karaca-Mandic’s research has linked ICU bed use to increased mortality.
“What the facility-level data is showing us is how localized the pandemic can be,” she said.
The U.S. West is grappling with some of the most acute repercussions. When scaled for population, Nevada and Arizona reported the highest hospitalization rates nationwide Monday.
Late-Night Calls
In Mesa, Arizona, about 20 miles east of Phoenix, Lee Allen passes families pressed against the windows of the hospital where he works as a nurse anesthetist. Some hold cardboard signs with words of encouragement.
Just inside, patients are being treated in the nearly full ICU, which has been expanded into under-used parts of the building. Many can’t read the signs as they lay face down to improve airflow to their lungs.
Though Allen’s primary specialty is obstetrical anesthesia, he has gotten more frequent calls for assistance with especially difficult intubations, such as for patients who have co-morbidities or are morbidly obese. Just a few days ago, he was called in at 2 a.m.
“I’m hopeful that the vaccine is going to help out,” said Allen, who is immunocompromised himself and got the vaccine on Monday.

In neighboring California, the virus has exploded with renewed fury. Cases, hospitalizations and deaths all smashed records last week.
Governor Gavin Newsom said Monday the state could see more than 90,000 people hospitalized with Covid-19 by mid-January, if the current surge doesn’t slow down. California reported a record 18,359 Covid patients in its hospitals Monday, a 67% increase in two weeks. ICUs in Southern California and the San Joaquin Valley are effectively full, and just 2.5% of the entire state’s ICU capacity remains open. The state has lost 2,741 people to the coronavirus in the last two weeks alone.
“Some counties or some regions may begin to exceed their existing, stated hospital capacity -- not just ICU capacity -- by the end of the month and in early January,” Mark Ghaly, secretary of California’s Health and Human Services agency, said during a news conference Monday. “We don’t see that across the entire state at that time, but we’re watching it very closely.”
California opened four temporary care facilities and has another seven ready if needed. Ghaly said hospitals have been making contingency plans to activate “crisis care teams,” which would make the difficult decisions of prioritizing care among sick patients should facilities become overwhelmed.
The state so far has been able to transfer patients from overloaded hospitals to those with more capacity, but that is becoming more difficult as the outbreak grows, he said.
Even though bed availability is tight in certain parts of the country, bottlenecks often stem more from staffing constraints. Those with coronavirus are more time consuming, costly and labor-intensive than typical patients.
“We can’t really downplay the emotional strain,” said Ann-Marie Alameddin, president and chief executive officer of the Arizona Hospital and Healthcare Association, where hospital bed occupancy is estimated at 78% statewide. “I think there’s going to be lasting effects that we’ll be navigating for months and years to come.”
The persistence of the Covid-19 crisis has worn down the health-care workforce. While much of the public has moved on from the April period when they stayed home and clapped for medical workers, “for many of our providers, that workload, those 13-hour days haven’t really stopped,” said Andy Brailo, chief customer officer at Premier Inc., which provides purchasing, technology and consulting services to more than 4,000 hospitals.
Attrition Surge
Premier’s clients have watched attrition spike, on average seeing turnover of 30% among clinical staff during the last few months, Brailo said. Some workers are retiring or shifting to part-time status. Others have been sidelined temporarily for illness or exposure to Covid-19, or must stay home to take care of children or family.
Health systems are boosting bonuses and overtime pay to recruit and retain staff, as well as reaching out to retirees. Demand for travel clinicians who take temporary assignments is extremely high.
More sophisticated care and treatments, like Regeneron Pharmaceuticals Inc.’s antibody cocktail, have improved the outlook for patients who end up in hospitals. In New York, patients are moving through the hospital faster and a smaller ratio require intensive care and intubation.
As hospitals fill up, some people who might normally have been admitted for Covid-19 or other conditions get sent home instead, said Ashish Jha, dean of the Brown University School of Public Health.
The strain on capacity could lead to worse outcomes particularly for people whose conditions are borderline -- not so critical that they must be admitted immediately, but not so mild that they wouldn’t benefit from hospital care.
“Every bit of data suggests that a lot of those people aren’t going to do as well,” Jha said. They may get better, or return to the hospital sicker later on, or even die at home. “When you get into crowding situations, when emergency departments get overwhelmed or when hospitals get really full, everybody tends to do a little bit worse.”
©2020 Bloomberg L.P.