Doctors Fear Arizona Virus Overload as Hospital Cases Top N.Y.
Doctors Fear Arizona Virus Overload as Hospital Cases Top N.Y.
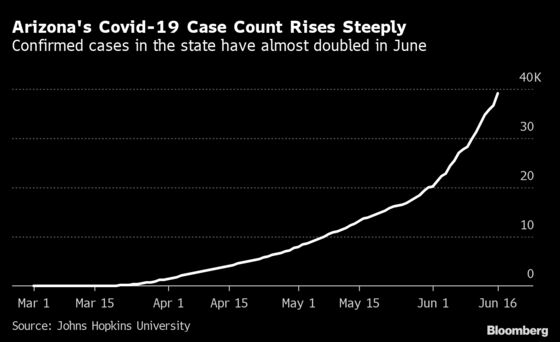
(Bloomberg) -- A surge in Covid-19 cases and hospitalizations in states including Arizona, Texas and Florida is showing signs of straining health systems and increasing concern about how officials will respond to a new wave of infections after loosening lockdowns.
While some data points are encouraging — the case count nationally has dropped to a daily increase of about 1%, new fatalities have declined, and virus tests are far more plentiful, as is the personal protective equipment vital for safeguarding front-line workers caring for the sick — states like Texas and Florida report persistent increases in hospitalizations and cases weeks into their reopening.
In New York, once the epicenter of the U.S. outbreak, the daily death count fell to 17 on Wednesday, down from a high earlier this year of 799. New cases rose just 0.1%.
In Arizona, where coronavirus cases and hospitalizations are rising to the alarm of experts, hospitals still face a critical limitation: staff. Arizona reported its highest number of hospitalized Covid-19 patients, 1,582 on Tuesday, a count that for the first time exceeds New York. While health-care facilities have stocked up on supplies and made plans to manage an influx of patients, a deficit of doctors and nurses can't be readily repaired.
Other U.S. hospitals could face similar staffing crunches in the months ahead as the pandemic spreads.
Murtaza Akhter is a clinical assistant professor in emergency medicine at the University of Arizona College of Medicine – Phoenix who works at multiple Arizona hospitals. On his emergency-room shift on Monday, he said he saw a dramatic difference over the previous week in the number of people, respiratory patients, and positive tests.
“I was quite taken aback,” Akhter said. “It could fairly easily tip over.”
Health-care providers fear they'd have no chance of coping with an influx of patients akin to the one faced by New York City hospitals. There, more than 53,600 individuals have been hospitalized with the virus, forcing the construction of hospital tents in Central Park, the repurposing of a convention center and the loan of a U.S. Navy hospital ship to try to find enough resources to treat patients.
Steven Oscherwitz, an infectious-disease specialist in Arizona, said that when he visited Tucson Medical Center on Monday morning, there was just one ICU bed available. Patient demographics have also changed since he first started seeing virus patients. “Now the younger ones are coming, and it’s in the community more than just nursing homes,” he said.
Oscherwitz predicted that hospitals will soon be so strained that they’ll have to “ration care” and triage patients. “We’re just not prepared,” he said.
Governor Doug Ducey meanwhile said last week that Arizona has capacity despite the rise in cases. The state is “not seeing an increase in patient volume,” he said, but “we are prepared if that increase should come.”
Read More:
-
Oregon Joins Florida, Texas in Confronting Covid-19’s Resurgence
-
Lone Doctor Fights NYC-Style Covid Outbreak in U.S. Black Belt
-
Behind Florida’s Covid-19 Surge: What the Charts Are Showing
Roy Boukidjian, system vice president of infection prevention for CommonSpirit Health, a Catholic health-care system that operates hospitals throughout the country including Dignity Health in Arizona, said they’re better prepared than during the first wave. In Washington and California, where some of the first clusters of cases appeared in the U.S., “we were building the plane as we flew it.”
The virus is completely unlike other disasters facilities prepare for like gun violence and natural disasters, said Lindsay Lief, an assistant professor in the division of pulmonary and critical care at Weill Cornell Medicine in New York. The biggest challenge isn’t equipment but trained staff, which “you can’t just buy more of. FEMA can’t just send it to you. ICU nurses can’t just be created overnight,” she said.

New York City had the benefit of being the focus of the country’s attention. Medical volunteers from around the country traveled there to help their colleagues. With the new spikes spread across more states, coming months into the battle with the new virus, Lief said that sort of support isn’t likely.
“It’s going to be much harder this time,” Lief said. “If there are five states that need help at once, and a bunch of other states are either preparing for things to get worse or recovering from a bad surge, I can’t imagine there’ll be the outpouring there was for us.”
Banner – University Medical Center Phoenix’s 120-bed intensive care unit is nearly full and several nurses short, according to critical-care specialist and pulmonologist Jennifer O’Hea. The ICU is turning away patients transferred from other state health facilities and the health system brought several nurses in from Colorado to help.
“I worry every day if the shift I’m about to go into is the day I can’t give the care I know is adequate,” O’Hea said.
About 20 miles from the Mexico border, the 406-bed Yuma Regional Medical Center was about two-thirds full on Tuesday. Less than half were there for Covid-19, according to President and Chief Executive Officer Robert Trenschel. Sixteen of the ICU’s 42 beds were taken by virus patients, leaving him feeling okay.
Staffing is Trenschel’s concern, he said. It’s begun pulling nurses from other parts of the organization to help in the ICU, limited or postponed elective surgeries to free up staff and beds, and used Arizona’s surge line to help coordinate patient transfers to avoid being overloaded, he said.
Little Social Distancing
Robert Raschke, a critical care physician at HonorHealth Scottsdale Osborn Medical Center, said that since March or April, the Covid-19 caseload “sort of plateaued, and is now going up significantly.” There are about 60 beds in the part of the ICU where he works, which are shared with trauma surgeons, Raschke said.
“The things we worried about back in April that we kind of avoided here in Arizona are happening now,” he said, like steady increases in patients coming into the ICU. When they get there, patients may stay for as long as a month. So “it doesn’t take a surge of cases to cause a great backlog of people,” he said.
Raschke also fears that state isn’t taking precautions like social distancing. He witnessed it firsthand the other week when he went to get takeout at a restaurant.
“‘I work in an ICU and it’s full of Covid patients, and no one in this place is wearing a mask but me. You guys have to believe me that it’s real,’” he said he told the waitress. “She said, ‘Have a nice day.’”
©2020 Bloomberg L.P.