Covid ‘Long Haulers’ Ask Who Pays When Sickness Just Won’t End
Covid ‘Long Haulers’ Ask Who Pays When Sickness Just Won’t End
(Bloomberg Law) -- (First of two parts)
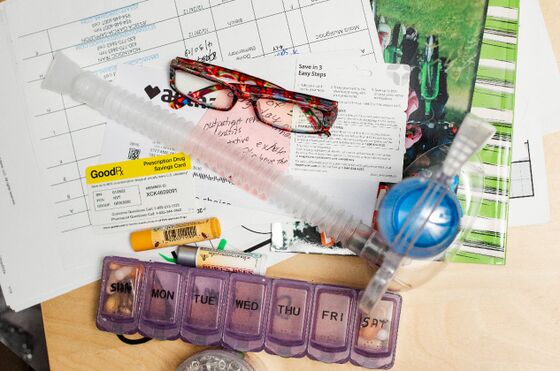
Stefanie Miller sounds like she’s rushing every word to take another breath.
Her voice is airy from vocal-cord damage, after 21 days on a ventilator that scarred her face. She’s battling extreme fatigue. Her joints ache. She’s losing her hair.
“No one knows how long it’s going to take for long-haulers to get over the symptoms,” said the 53-year-old second-grade teacher from Plantation, Fla., referencing the term for survivors whose illnesses just won’t go away.
Millions of people will live with coronavirus’s effects long after the pandemic subsides. Even mild cases have caused lung, heart and kidney damage in otherwise healthy people. It’s unclear what their future health-care needs will be, or how much their care will cost. As with HIV and opioid addiction crisis, the scope and newness of the pandemic presents many new questions about what treatments insurers will cover.
In this video, we explore the looming health insurance crisis for the millions of Americans who have contracted Covid-19. (Video by Andrew Satter; Executive Producer: Josh Block).
Group health plans and insurance companies are supposed to cover diagnostic testing for Covid-19 under federal laws passed in response to the pandemic. Plans shouldn’t charge deductibles, co-payments or coinsurance for office, telehealth, urgent care or emergency-room visits where a Covid-19 test is given or ordered.
But no federal law requires insurers to pay for coronavirus treatment.
“Insurers can put coverage limits on anything,” said Sara Rosenbaum, a professor of health law and policy at George Washington University. “It doesn’t matter if it’s Covid-related or not.”
It’s too early for a clear read on how insurers will deal with these long-hauler costs. Patients have to go through lengthy appeals processes with their insurance companies when a claim is denied, so disputes have yet to reach the courts.
The Affordable Care Act prohibits most health plans from refusing to cover people or hiking their costs if they have a pre-existing condition. But those safeguards could be wiped out if the Supreme Court strikes down or guts the ACA.
Even if Obamacare remains, insurance plans that fall under the law’s purview can decide what treatments are medically necessary and which doctors they’re willing to pay for. And its protections don’t apply to the short-term health plans expanded by President Donald Trump in a 2017 executive order.
A surge in claims relating to the virus’s long-term effects could cause out-of-pocket costs to soar if insurers create new coverage and treatment limits that include higher deductibles and coinsurance.
“The problem is many of the normal exclusions that might be built into an insurance policy were not outlawed under the ACA. So for example, you could have health insurers saying, ‘We don’t cover treatments related to a public health pandemic,’” Rosenbaum said.

Treatment Costs
Donna Talla, 56, of Springfield, Va., is already battling UnitedHealthcare over its refusal to pay for a test her cardiologist ordered. Talla was diagnosed with Covid-19 and admitted to Inova Fairfax Hospital with bilateral pneumonia on March 31. UHC, in its determination letter, said the test wasn’t medically necessary.
The virus, which put her in the hospital three more times over the next four months, caused a pulmonary embolism, a rapid heart rate, fatigue and hair loss. A UnitedHealthcare spokesperson said the company press office can’t look into the disputed bills or provide a comment unless Talla signs a waiver authorizing the release of her health information. Talla declined to sign the form.
The spokesperson did say that UnitedHealthcare, part of UnitedHealth Group Inc., voluntarily extended no-cost coverage for members receiving treatment for Covid-19. That policy was extended through Oct. 22, according to the company’s website.
“This coverage applies to members enrolled in Medicare Advantage, Medicaid and Individual and Group Market Health plans and we continue to review state and federal guidance to ensure our policies are consistent with recent guidelines,” the UHC spokesperson said in a statement. “With regard to ongoing health care coverage, we cover care according to the member’s benefit plan and if a member or provider has questions, we encourage them to contact us so that we can assist them.”

In a statement, America’s Health Insurance Plans (AHIP) said, “Health insurance providers are committed to improving access to safe, timely, affordable, appropriate care, including for those who have overcome COVID-19 and are dealing with its long-term impact on their health, using the best evidence science can offer.”
Comparable Coverage
Even with protections for pre-existing conditions, any treatment or procedure for a condition stemming from Covid-19 has to meet certain clinical criteria for insurers to cover it as medically necessary.
“When you have new treatments for new conditions, they aren’t always proven yet,” said Leslie Moran, senior vice president of the New York Health Plan Association, which represents 28 plans statewide.
Early research suggests there may be long-term heart, lung, and kidney damage even in healthy young people who recover from Covid-19, said Dr. Emily Landon, chief health-care epidemiologist at the University of Chicago Medicine.
Anxiety, post traumatic stress and depression are other long-term effects that could spur disputes with insurers.
Individual- and small-group health plans have to cover mental health and substance use treatment under the ACA. Large employer health plans, those with over 50 employees, aren’t required to offer that benefit, but if they do it has to be comparable to the coverage of physical health care.
The definition of what’s medically necessary and how it’s applied to decisions on what care is covered gives insurers and health plans broader discretion to deny mental health and substance use services, said JoAnn Volk, research professor at the Georgetown University Center on Health Insurance Reforms.
In addition to her primary-care doctor; physical, occupational and speech therapists; pulmonologist; ear, nose, and throat doctor; and neurologist, Miller sees a therapist for anxiety and post-traumatic stress.
While on the ventilator in a medically-induced coma during April and May, she experienced vivid and terrifying delusions. She said going back to the doctor triggers the feelings of fear and isolation she experienced.
“It gets me so jolted and upset,” Miller said. “The noises remind me of the hospital.”
Pre-existing Condition Protections
More than 23 million people could lose their insurance If the ACA is outlawed, the Center for American Progress estimates. A group of Republican-led states and the Justice Department are urging the Supreme Court to overturn the law, arguing it can’t survive after a provision requiring everyone to buy health insurance was declared unconstitutional.
“People who have had Covid-19 may have trouble in the future getting coverage, or getting coverage for anything that stems from the long-term effects of Covid,” said Cori Uccello, senior health fellow at the American Academy of Actuaries.
The ACA defines pre-existing conditions as any health problem a person had before starting new coverage. Each insurer decided what counted and what didn’t prior to the law’s enactment. The ACA expanded on the limited safeguards under the 1996 Health Insurance Portability and Accountability Act (HIPAA) that prohibited insurers from denying coverage when someone is changing jobs and switching employer-sponsored health plans.
HIPAA never regulated premiums and did little to protect people who lost their job-based coverage, like the nearly half-million people who signed up for Obamacare outside of the open enrollment period from mid-December to May.
“HIPAA didn’t do very much for people who needed to buy their health insurance on their own, ” said Karen Pollitz, senior fellow on health reform and private insurance at the Kaiser Family Foundation.
As of October 2019, only 12 states have passed their own laws to keep the ACA’s protections for pre-existing conditions regardless of what happens to the federal statute, according to data provided by Georgetown researchers.
Insurer Concerns
So far, coronavirus has been immensely profitable for insurers. Postponed elective surgeries and other health care that people didn’t seek during the pandemic resulted in fewer claims for insurers to pay, but they don’t expect that to continue.
AHIP estimated treatment costs for Covid-19 could range from $30 billion to $547 billion over the next two years. But the group AHIP hired for the study didn’t include in their model the long-term costs associated with Covid survivors, so the estimate could be an undercount.
A report the Urban Institute compiled with Georgetown researchers, after interviewing executives from 25 insurance companies, cited their concerns that the pandemic could lead to more consolidation among health providers who then demand more money “as larger practices and health systems gain greater negotiating leverage.”
Insurers told researchers they’re also worried about cash-strapped small businesses dropping health plans entirely since “a higher number of small employer clients than usual are already in payment delinquency.”
People left without job-based coverage are likely to turn to Medicaid if they can’t afford insurance through federal or state exchanges. Enrollment in Medicaid and the Children’s Health Insurance Program jumped from 71.5 million in March to 74.6 million in June, according to the latest data available from the Centers for Medicare and Medicaid Services.
‘Completely Compromised’
So far this school year, Broward County Public Schools has relied solely on distance learning. Miller teaches her 18 second graders at Fox Trail Elementary from home from 7:30 a.m. to 3 p.m. during the week. Even that’s a struggle.
“I’m tired,” she said. “All teachers are exhausted right now trying to figure this out. Being in my condition, it’s even more challenging.”
She’s worried much of the summer about when she’ll be required to go back to her classroom. Now that may become a reality. The Broward County Public School Board voted last week to start bringing students and teachers back for in-person instructions under a gradual re-opening plan that begins Oct. 9.
Miller asked for an accommodation to continue teaching remotely and will continue working from home while waiting for a decision. She sees it as a matter of life and death.
“My lungs are completely compromised,” she said. “If I get it again I could die.”
Tomorrow: How Covid-19 alters employment.
—With assistance from Sara Hansard.
To contact the reporter on this story: Lydia Wheeler in Washington at lwheeler@bloomberglaw.com
To contact the editor responsible for this story: Fawn Johnson at fjohnson@bloomberglaw.com
©2020 Bloomberg L.P.